Understanding Cancer Genetics and Life Expectancy with HER2
Cancer is a complex group of diseases characterized by the uncontrolled division and growth of abnormal cells. Among the various types of cancer, understanding the genetic factors that contribute to its development is crucial for effective diagnosis and treatment. HER2, or human epidermal growth factor receptor 2, is a key player in the genetics of certain cancers, particularly breast cancer. In this article, we delve into the significance of HER2 in cancer genetics and its implications for life expectancy.
The Role of HER2 in Cancer
HER2 is a gene that provides instructions for making proteins involved in the growth and division of cells. Normally, these proteins help regulate cell growth, but in some cases, genetic mutations can cause the overproduction of HER2 proteins. This overexpression can lead to uncontrolled cell growth and division, contributing to the development and progression of cancer.
Breast cancer is one of the cancers where HER2 plays a significant role. Approximately 15-20% of breast cancers are HER2-positive, meaning they overexpress the HER2 protein. HER2-positive breast cancers tend to be more aggressive and have a higher likelihood of spreading compared to HER2-negative breast cancers.
HER2 and Treatment Strategies
Understanding the HER2 status of a cancer is crucial for determining the most effective treatment strategies. HER2-positive breast cancers are often treated with targeted therapies, such as trastuzumab (Herceptin), which specifically target the HER2 protein. These targeted therapies have revolutionized the treatment landscape for HER2-positive breast cancer, improving outcomes and reducing the risk of recurrence.
In addition to targeted therapies, HER2 status also influences the choice of other treatments, such as chemotherapy and hormone therapy. Tailoring treatment plans based on the genetic profile of the cancer allows for more personalized and effective interventions.
Impact on Life Expectancy
The HER2 status of a cancer can have implications for life expectancy. HER2-positive breast cancers, if left untreated or not properly managed, may have a poorer prognosis compared to HER2-negative breast cancers. However, advancements in targeted therapies and personalized medicine have significantly improved the outlook for individuals with HER2-positive breast cancer.
Early detection and timely intervention play a crucial role in improving life expectancy for individuals with HER2-positive breast cancer. Regular screening, awareness of risk factors, and advancements in genetic testing contribute to identifying HER2 status early in the diagnostic process.
Research and Future Directions
Ongoing research in cancer genetics, including the study of HER2, continues to provide insights into the development of new therapies and treatment approaches. Scientists are exploring ways to further refine targeted therapies and identify additional genetic factors that may influence cancer progression.
Additionally, understanding the interplay between genetics and environmental factors is essential for a comprehensive understanding of cancer development. Lifestyle factors, such as diet, exercise, and exposure to environmental toxins, can interact with genetic predispositions, influencing the overall risk and prognosis of cancer.
In conclusion, unraveling the mysteries of cancer genetics, particularly the role of HER2, has significantly enhanced our ability to diagnose and treat cancer effectively. The advent of targeted therapies has brought about a paradigm shift in cancer treatment, positively impacting the life expectancy of individuals with HER2-positive breast cancer.The field holds promise for further advancements that will continue to improve outcomes and quality of life.
Challenges and Triumphs in HER2-Positive Breast Cancer
While the progress in treating HER2-positive breast cancer is remarkable, challenges still exist. Resistance to targeted therapies can develop over time, leading to disease recurrence. Researchers are actively investigating mechanisms of resistance to develop strategies to overcome this hurdle. Clinical trials are ongoing to test new drugs and combinations, aiming to further improve outcomes for individuals with HER2-positive breast cancer.
One notable area of exploration is immunotherapy. Harnessing the body’s immune system to target and destroy cancer cells has shown promise in various cancers, and researchers are exploring its potential in HER2-positive breast cancer. Combining immunotherapy with existing targeted therapies could offer a more comprehensive approach to treatment.
Moreover, the impact of HER2 extends beyond breast cancer. HER2 is also relevant in other cancers, such as gastric cancer, where HER2-positive tumors have been identified. Understanding the commonalities and differences in HER2’s role across various cancer types is crucial for developing broader treatment strategies.
Genetic Counseling and Testing
Given the importance of HER2 in cancer genetics, genetic counseling and testing play a vital role, especially for individuals with a family history of breast cancer or those diagnosed at a younger age. Genetic testing can identify mutations in the HER2 gene and other cancer-related genes, providing valuable information for treatment decisions and informing family members about potential risks.
Genetic counseling helps individuals and their families understand the implications of genetic test results, addressing emotional and ethical considerations. It empowers individuals to make informed decisions about their healthcare and take steps to manage their cancer risk.
Lifestyle Factors and Prevention
While genetics play a significant role in cancer development, lifestyle factors also contribute to overall cancer risk. Adopting a healthy lifestyle, including a balanced diet, regular exercise, and avoiding tobacco and excessive alcohol consumption, can contribute to cancer prevention and overall well-being.
Regular screenings and early detection remain crucial, particularly for individuals with known genetic predispositions. Early intervention can significantly impact treatment outcomes and life expectancy. Moreover, advances in imaging technologies and screening methods continue to enhance our ability to detect cancer at earlier, more treatable stages.
Empowering Patients and Advocacy
Empowering patients with knowledge about their cancer, treatment options, and the role of genetics is essential. Support groups, patient advocacy organizations, and online communities provide valuable resources and a platform for individuals to share experiences and information.
Advocacy efforts also play a pivotal role in driving research, raising awareness, and influencing policy changes. Increased funding for cancer research, improved access to genetic testing, and enhanced support for patients undergoing treatment are critical components of a comprehensive approach to cancer care.
Understanding cancer genetics, particularly the role of HER2, has transformed the landscape of cancer diagnosis and treatment. Advances in targeted therapies have significantly improved outcomes for individuals with HER2-positive breast cancer, marking a triumph in the field of oncology. Ongoing research, coupled with genetic counseling, lifestyle interventions, and advocacy, contributes to a holistic approach to cancer care.
As we continue to unravel the complexities of cancer genetics, collaboration between researchers, healthcare professionals, and patients remains essential. The journey conquering cancer involves not only scientific breakthroughs but also a collective effort to support and empower those affected. By fostering a multidisciplinary approach, we move closer to a future where the impact of cancer is minimized, and the prospects for a longer and healthier life for all individuals become a reality.
The Future of Cancer Genetics and Personalized Medicine
Looking ahead, the future of cancer genetics holds exciting prospects for personalized medicine. As our understanding of individual genetic variations deepens, tailoring treatments to the specific genetic profile of each patient becomes increasingly feasible. This approach, known as precision medicine, aims to optimize therapeutic strategies, minimize side effects, and enhance overall treatment efficacy.
Advancements in genomic sequencing technologies are paving the way for more comprehensive genetic profiling. Whole-genome sequencing and other high-throughput techniques enable researchers and clinicians to analyze a patient’s entire genetic makeup, providing a wealth of information beyond individual genes like HER2. This broader perspective allows for a more nuanced understanding of the intricate interplay between genetic factors in cancer development.
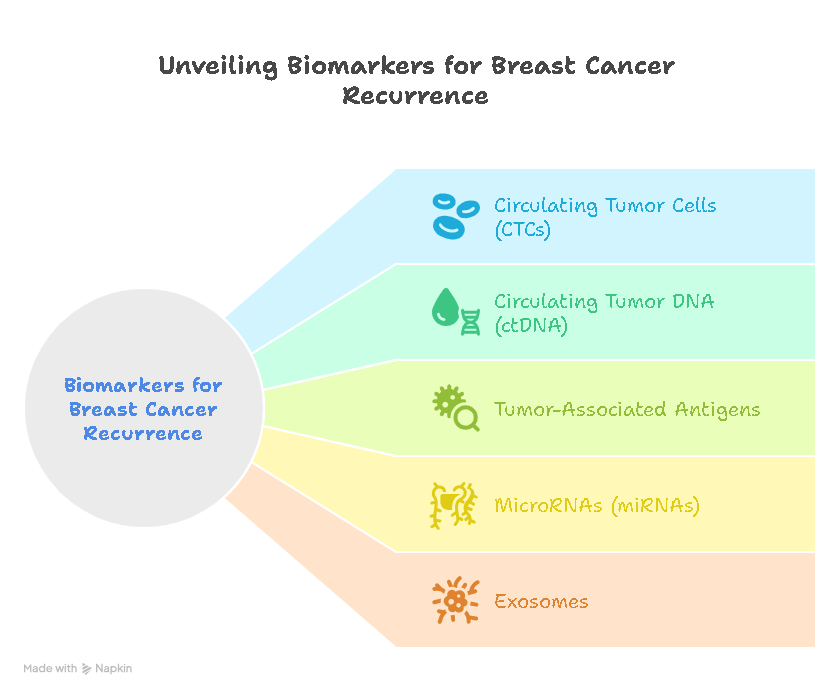
The concept of liquid biopsies, which involve analyzing circulating tumor DNA in the bloodstream, is gaining momentum. This non-invasive approach provides real-time information about the genetic makeup of tumors, offering a dynamic view of cancer evolution. Liquid biopsies hold promise for monitoring treatment response, detecting early signs of resistance, and adjusting treatment plans accordingly.
Collaboration between researchers, pharmaceutical companies, and healthcare providers is essential for translating scientific discoveries into tangible benefits for patients. Clinical trials exploring novel therapeutic agents and combination treatments continue to expand, providing avenues for testing cutting-edge interventions that may further revolutionize cancer care.
Ethical Considerations and Equitable Access
As the field of cancer genetics advances, ethical considerations surrounding genetic information become increasingly pertinent. Striking a balance between the potential benefits of genetic testing and the ethical implications of privacy, consent, and discrimination is crucial. Robust frameworks and guidelines are essential to ensure responsible and equitable use of genetic information in clinical practice.
Equitable access to genetic testing and cutting-edge treatments is another imperative. Disparities in healthcare access can exacerbate existing inequalities, limiting the benefits of advanced genetic technologies to certain populations. Advocacy for policies that promote inclusivity and ensure access to state-of-the-art cancer care for all individuals, regardless of socioeconomic status, is integral to the future of cancer medicine.
Educating Healthcare Professionals and the Public
As the landscape of cancer genetics evolves, educating healthcare professionals becomes paramount. Ensuring that clinicians are well-versed in the interpretation of genetic data, the latest treatment modalities, and the nuances of personalized medicine is essential for delivering optimal patient care.
Public awareness and education also play a vital role in empowering individuals to make informed decisions about their health. Demystifying complex genetic concepts, dispelling myths, and fostering an understanding of the implications of genetic testing contribute to a more informed and engaged patient population.
In conclusion, the journey into the depths of cancer genetics, epitomized by the role of HER2, is an ever-evolving narrative. The triumphs achieved in understanding and treating HER2-positive breast cancer exemplify the potential of genetic insights to transform lives. With ongoing research, ethical considerations, and a commitment to equitable access, the future holds promise for a paradigm shift in cancer care—a future where precision medicine becomes the norm, and the individual genetic blueprint guides tailored, effective treatments, ultimately extending and improving the lives of those affected by cancer.
Empowering Patients through Genetic Literacy
As we navigate the intricate landscape of cancer genetics, empowering patients with genetic literacy becomes essential. Education campaigns geared toward patients and their families can help demystify complex genetic concepts, enabling them to actively participate in their healthcare decisions. Understanding the significance of HER2 and other genetic markers fosters a sense of empowerment, allowing individuals to advocate for themselves and make informed choices about their treatment plans.
Patient support networks and advocacy organizations play a pivotal role in disseminating accurate information, providing a platform for shared experiences, and offering emotional support. These networks create a sense of community, helping patients and their loved ones navigate the challenges of a cancer diagnosis while staying informed about the latest developments in cancer genetics.
Technological Advancements and Data Security
As technology continues to advance, the integration of artificial intelligence (AI) and machine learning into cancer genetics research holds great promise. These technologies can analyze vast amounts of genetic data, identify patterns, and contribute to the discovery of novel therapeutic targets. However, the ethical use of AI in healthcare, ensuring data security, and protecting patient privacy are paramount considerations that require ongoing attention.
The establishment of robust data-sharing frameworks facilitates collaboration among researchers and institutions, accelerating the pace of discovery. Simultaneously, strict data protection measures must be in place to safeguard sensitive genetic information. Striking a balance between collaboration and privacy is crucial to maintaining public trust and advancing scientific knowledge.
Global Collaboration and Knowledge Sharing
Cancer knows no borders, and the complexities of cancer genetics demand a global collaborative effort. International partnerships among researchers, healthcare professionals, and policymakers are instrumental in pooling resources, sharing insights, and addressing the diverse genetic landscapes present in different populations.
Global collaboration also extends to ensuring equitable access to genetic testing, treatments, and information. By fostering an environment of knowledge sharing and cooperation, the international community can work toward reducing disparities in cancer outcomes and improving the overall quality of cancer care worldwide.
The genetic alterations detected in your breast tumor play a crucial role in determining your prognosis and guiding your medical team in recommending the most optimal treatment approach. Breast cancer cells classified as HER2-positive exhibit elevated levels of the HER2 protein, which stimulates cell growth. Typically, HER2-positive breast cancer cells demonstrate a tendency to proliferate and metastasize rapidly. However, advancements in treatment options, particularly targeted therapies, are positively impacting life expectancy outcomes for individuals with this subtype of breast cancer.
The Ongoing Evolution of Cancer Care
In the ever-evolving realm of cancer care, staying informed about the latest research and treatment options is crucial. Healthcare providers must remain at the forefront of advancements in cancer genetics to deliver the best possible care to their patients. Continuing education, professional development, and interdisciplinary collaboration contribute to a comprehensive and evolving understanding of cancer biology.
Patients, too, can benefit from staying informed about ongoing research, clinical trials, and emerging therapies. Open communication between healthcare providers and patients fosters a collaborative approach to treatment, where shared decision-making becomes a cornerstone of care.
In conclusion, the journey into understanding cancer genetics and the role of HER2 is a multifaceted exploration with profound implications for patients, healthcare providers, and researchers alike. As we forge ahead, the synergistic interplay of scientific discovery, ethical considerations, and global collaboration will shape the future of cancer care. Together, we aspire to a future where the intricacies of cancer genetics are unravelled, and where each individual’s unique genetic makeup guides personalized, effective, and compassionate cancer treatments.
Patient-Centric Care: A Vision for the Future
In envisioning the future of cancer care, a patient-centric approach takes center stage. As we delve deeper into the intricacies of cancer genetics, the emphasis on tailoring treatments to the individual becomes more pronounced. Genetic information, including HER2 status, acts as a guide for personalized treatment plans, allowing healthcare providers to offer interventions that are not only effective but also aligned with each patient’s unique genetic makeup.
The concept of patient-reported outcomes gains prominence in this vision for the future. By incorporating patients’ perspectives on their quality of life, treatment tolerability, and overall well-being, healthcare providers can fine-tune interventions to better align with individual preferences and needs. Patient engagement in decision-making, supported by robust communication between healthcare teams and patients, fosters a collaborative and empowering healthcare environment.
Preventive Strategies and Early Intervention
As our understanding of cancer genetics advances, preventive strategies gain momentum. Genetic testing for high-risk individuals and those with a family history of cancer allows for proactive interventions, such as increased surveillance or risk-reducing surgeries. Identifying individuals at elevated risk based on their genetic profile empowers them to make informed decisions about their health and take preventive measures to mitigate their cancer risk.
Furthermore, early intervention remains a cornerstone of improved cancer outcomes. Enhanced screening technologies, coupled with genetic insights, enable the detection of cancer at its earliest, most treatable stages. Integrating genetic information into routine screenings contributes to a more comprehensive and personalized approach to early cancer detection.
Education as a Catalyst for Change
Educating the next generation of healthcare professionals, researchers, and the public is integral to shaping the future of cancer care. Academic institutions and training programs should incorporate the latest advancements in cancer genetics into their curricula, ensuring that future healthcare providers are well-equipped to navigate the complexities of personalized medicine.
Public awareness campaigns, educational initiatives, and community outreach programs contribute to a more informed society. A population that understands the importance of genetic testing, recognizes the signs of cancer, and actively engages in preventive measures is better equipped to contribute to the overall success of cancer prevention and treatment efforts.
Innovation and Continuous Research
The future of cancer care hinges on a commitment to innovation and continuous research. Investments in cancer genetics research, clinical trials, and the development of cutting-edge technologies are essential to unraveling the remaining mysteries of cancer and refining treatment strategies.
Collaborative platforms that facilitate the exchange of ideas, data, and resources across institutions and countries contribute to a more accelerated pace of discovery. The frontiers of cancer genetics must be supported by a framework that encourages creativity, collaboration.
Cancer begins when the genes in a cell develop certain types of mutations. Knowing which mutations your breast cancer cells carry will help you and the rest of your cancer care team understand your condition better.
Conclusion: A Unified Vision
In conclusion, the journey into cancer genetics, epitomized by the exploration of HER2, marks a transformative chapter in the narrative of cancer care. The future holds the promise of more effective, personalized treatments, early detection strategies, and a comprehensive understanding of the genetic underpinnings of cancer.
By embracing patient-centric care, prioritizing preventive measures, fostering education, and a future where the impact of cancer is minimized, where personalized treatments based on genetic insights are the norm, and where the journey from diagnosis to survivorship is marked by compassion, empowerment, and scientific triumphs. The ongoing collaboration of patients, healthcare professionals, researchers, and advocates is the catalyst for realizing this vision and transforming the landscape of cancer care for generations to come.











Leave a Reply